Malignant hypertension and hyperreninemia: primary or secondary hypertension? A case report
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
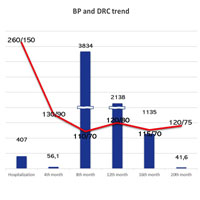
Malignant hypertension is a rare condition characterized by severe hypertension and multi-organ ischemic damage. Marked activation of the renin-angiotensin system is observed in many patients, but its persistence over time is not known. We report a case of a 42-year-old woman who presented with severe hypertension and multi-organ damage. Initial evaluation showed an elevated value of direct renin concentration with normal plasma aldosterone concentration and a nodular lesion in the left adrenal gland. The differential diagnosis between the primary and secondary form of hypertension had to be questioned. Consequently, the patient was followed up for 20 months. Repeated checks showed a significant increase in renin levels with a normal aldosterone concentration and regression of organ damage. After 20 months, renin values returned within normal range. Hyperreninemia persisting over a long period of time has not been fully explained. Long-term follow-up allowed us to attribute malignant hypertension to de novo essential hypertension.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.






