A case of hemolytic anemia associated with interstitial lung disease, arthralgia and fever caused by Mycoplasma pneumoniae
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
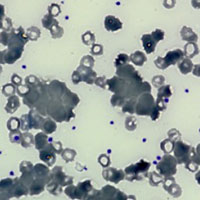
Pulmonary interstitiopathies became the most diagnosed forms of pneumonia in 2020 due to the coronavirus (COVID-19) pandemic. The spectrum of interstitiopathies is broad and includes idiopathic diseases and secondary forms. In April 2020, a 36-year-old man was admitted to our department for arthralgias, fever, asthenia, cough, and dyspnea. In January 2020, fever, cough, arthralgias, and asthenia appeared. In April, his general condition worsened with the development of macrohematuria, malaise, and intense asthenia. On admission, the patient presented pale, asthenic, and symptomatic for dyspnea and arthralgias. There was objective joint pain in the small joints of the hands, elbow, and knees with morning stiffness and decreased strength. Computed tomography of the chest documented ground-glass opacities in both lung fields. He performed 2 swabs for severe acute respiratory syndrome-related coronavirus 2, which were negative. On hematochemical examination: immunoglobulin (IgM) 332 mg/dL and ferritin 700.2 ng/mL. At venous blood smear peripheral venous blood, agglutination of erythrocytes. The serology (IgM) for Mycoplasma pneumoniae was positive with agglutinins in the serum; doxaciclina was started. There was a progressive normalization of hemoglobin levels, cold agglutinins were gradually reduced and were no longer detected at 15 days after the start of treatment. At one month after discharge, pulmonary function had fully recovered, and the picture of hemolytic anemia was resolved.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.






