Epicardial fat, gender, and cardiovascular risk
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
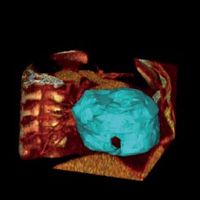
Epicardial fat (EF) is considered an important risk factor and an active player in the pathogenesis of cardiovascular and metabolic diseases. EF is an endocrine organ that releases hormones and mediators, including the circulating C-reactive protein (CRP), and plays a vital role in modifying the vascular endothelial function and promoting the growth of coronary atherosclerosis. This study aimed to investigate the relationship between CRP concentrations and EF in a cohort of patients with metabolic syndrome at risk for coronary artery disease. In our study, carried out in primary prevention, we enrolled 36 subjects (M/F: 21/15; age: 59.3±0.79 yrs) diagnosed with metabolic syndrome. We have classified the patients into two groups: Men and Women. Besides anthropometric characterization and screening laboratory tests, the subjects performed a multidetector computed tomography scan, which allowed the EF quantification. Mean EF was 115.1 cc in the study population. The average EF of women was 111 cc; the average EF of men was 118 cc (P=0.18). CRP levels were strongly positively correlated with EF area in women (P=0.01), while the correlation was not found in men (P=0.4). Our findings suggest that, in women, the EF produces a greater amount of acute-phase proteins and increases the pro-inflammatory state in the epicardial region. For this reason, we can hypothesize, in women, a different role in the development of atherosclerotic plaque of the epicardial fat compared to men.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.






