Association of methionine synthase reductase (MTRR A66G) polymorphism with susceptibility to acute lymphoblastic leukemia
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
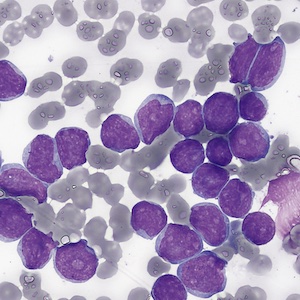
Background and Objectives. The enzyme methionine synthase reductase is involved in cellular methylation reactions, DNA synthesis, and epigenetic processes. It is encoded by the MTRR gene, which garnered a lot of attention in current medical genetics research. This study was conducted to study the association between MTRR (A66G) polymorphism and the risk of developing acute lymphoblastic leukemia among Sudanese patients. Materials and Methods. This is a case-control study in which 150 patients with acute lymphoblastic leukemia (ALL) and 150 healthy participants as a control group were enrolled. DNA was extracted and analyzed for the MTRR (A66G) polymorphism using the real-time polymerase chain reaction. Results. Based on flow cytometry results, B-ALL was more common (79%) than T-ALL (21%). The comparison of hematological parameters in acute lymphoblastic leukemia subtypes showed a statistically significant high mean total white blood count (P=0.000) and mean blast percentage (P=0.050) in patients with T-ALL. The molecular analysis showed that the incidence of the MTRR homozygous genotypes AA and GG were higher in the patients (44% and 9.3%, respectively) compared to the control group (40% and 6.7%, respectively). In comparison, the heterozygous genotype AG was lower in the patients (46.7%) than in the control group (53.3%). However, the association between the polymorphism and acute lymphoblastic leukemia risk was not statistically significant (OR: 1.179, 95% CI 0.7459-1.865, P=0.445). Conclusions. This study concluded that MTRR A66G polymorphism was not associated with the risk of acute lymphoblastic leukemia among the Sudanese population.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.






