Anemia and iron in internal medicine: an Italian survey and a review on iron intravenous therapy in medical patients
HTML: 84
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
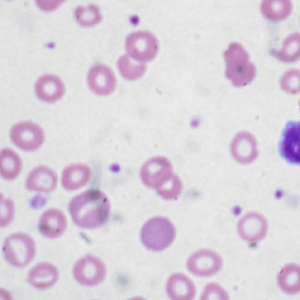
Authors
In Italy, Internal Medicine Units hospitalize approximately 1,300,000 patients, often elderly and comorbid. The prevalent diagnoses are respiratory diseases, heart failure, or pneumonia. As a matter of fact, anemia is probably underestimated in the compilation of the official discharge forms (SDO) according to ICD-9 diagnostic codes. We promoted a survey among the Members the Italian Scientific Society of Internal Medicine (FADOI) with the aim to investigate the prevalence of anemia and iron deficiency, over than certain aspects related to the therapeutic management of patients with anemia. Furthermore, we performed a review summarizing current evidence for iron intravenous therapy in these patients. According to the survey, anemia is present in around half of the patients hospitalized in Internal Medicine, and about a quarter of them shows iron metabolism alterations. In the evaluation of iron metabolism, the dosage of ferritin is the most requested exam, whereas transferrin saturation is less considered. By focusing on some categories of patients, the awareness of the usefulness of intravenous iron therapy in patients with heart failure seems to be sufficiently common (76% of physicians), while it seems lower (60%) in the management of patients with chronic kidney disease (CKD) and anemia. Finally, more than 75% of the physicians answered that, in their hospital, there are few outpatients’ offices or diagnostic pathways dedicated to patients with anemia. Anemia due to absolute or functional iron deficiency is particularly prevalent in Internal Medicine inpatients. For this reason, an accurate evaluation of iron profile and an adequate iron therapy is mandatory in these patients. Recent studies show that, in patients with heart failure, intravenous iron therapy is an effective way of improving patients’ health, regardless of the presence of anemia. Similarly, iron therapy results fundamental to optimize erythropoiesis-stimulating agent efficacy in patients with chronic renal failure. In the next future, other therapeutic aspects of intravenous iron therapy will be probably clarified by several interesting ongoing studies focused on these patients.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.
Similar Articles
- Claudio Giumelli, Azio Reverzani, Riccardo Volpi, Giuseppe Chesi, Heart failure in real world , Italian Journal of Medicine: Vol. 9 No. 4 (2015)
- Mario Visconti, Proton pump inhibitors overuse: only inappropriate prescriptions or further iatrogenic damage? , Italian Journal of Medicine: Vol. 9 No. 3 (2015)
- Fernando Gallucci, Emiliana Marrone, Roberto Nappi, Maurizio Renis, Maria Gabriella Coppola, Tiziana Ciarambino, Daniele D’Ambrosio, Ada Maffettone, Maria D’Avino, CIN CIN for HF Group Researchers, Results of an observational retrospective multicenter study: “Campania INternal medicine - the Clinical INternist for heart failure” , Italian Journal of Medicine: Vol. 17 No. 1 (2023)
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/itjm.2022.1532
https://doi.org/10.4081/itjm.2022.1532



